Visual snow syndrome: the visual approach

This article is the result of a collaboration between our editorial team and the Visual Snow Initiative, an international nonprofit organization committed to raising awareness, educating and advocating for patients affected by Visual Snow Syndrome.
We are pleased to include the contribution of Sierra Domb, CEO of the organization, who enriches this discussion with her personal experience and specialized perspective.
Challenges with Visual Snow Syndrome
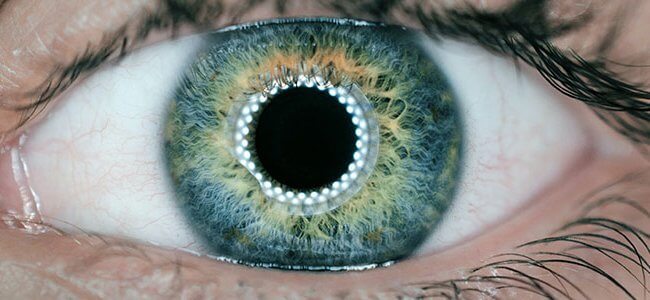
Visual Snow Syndrome (VSS) is a relatively recent neurological phenomenon that manifests as a continuous visual disturbance, characterized by full-field vision of numerous moving bright dots, resembling a real snow (so-called visual snow) or the static noise seen on an untuned television screen.
Visual snow syndrome has long been difficult to diagnose, often mistakenly attributed to eye-related problems, despite being a sensory processing disorder that affects the brain.
First mentioned in 1944 by ophthalmologist Frank D. Carroll1, it took years before VSS was recognized as a legitimate neurological condition.
The pathophysiology of VSS remains unclear, but previous research has shown that the condition involves alterations in several brain regions, including the temporal lobe, limbic system, and parietal lobe, which are associated with visual processing 2.
Although standard optometric and ophthalmologic tests typically yield normal results, VSS symptoms overlap with conditions such as migraine aura and Hallucinogen Persisting Perception Disorder (HPPD), often leading to misdiagnosis.
Unlike temporary visual disturbances, persistent visual snow is unique to VSS and remains present even with closed eyes.




Before scientific research clarified the condition, some considered it a supernatural phenomenon and feared they were going blind. Patients, already struggling with debilitating symptoms, were often dismissed, facing stigma that exacerbated their mental health, increasing anxiety, depression, dissociation, and even suicidal thoughts, in addition to the very real challenges they already endure.
Research indicates that VSS is not degenerative but can deeply impact quality of life, making daily activities such as reading, driving, working, attending school, or even recognizing landscapes and loved ones’ faces difficult due to excessive visual disturbances.3
The causes of the Syndrome
Although the exact cause remains unclear, literature suggests several possible triggers:
- Migraine: 51.7% of individuals with VSS have a history of migraines (van Dongen et al., 20194)
- Mild traumatic brain injury (mTBI): estimated in 20% to 40% of cases (Puledda et al., 20204)
- Hallucinogenic substance use (HPPD): Present in a minority of cases, generally less than 10 (Carroll, 19445).
Research funded by the Visual Snow Initiative (VSI) has been essential in obtaining recognition of VSS as a distinct condition. Inclusion in the ICD-11 (International Classification of Diseases) and ongoing studies on biomarkers, pathophysiology, and treatments are advancing understanding, improving diagnostics, and supporting accessible, safe, and scientifically backed therapeutic options.
Continuous awareness, education, and global collaboration are crucial to improving patient outcomes and care worldwide.
Diagnosis of visual snow syndrome
Visual snow syndrome (VSS) is diagnosed through a comprehensive clinical evaluation, including a detailed medical history and an eye examination to rule out other conditions, as optometric and ophthalmologic tests typically yield normal results.
In some cases, an MRI or EEG may be used to rule out other neurological conditions. VSS is typically diagnosed by exclusion, following the official diagnostic criteria developed by the Visual Snow Initiative.
Neuro-ophthalmologists, neurologists, ophthalmologists, orthoptists, optometrists, neuro-optometrists, and vision rehabilitation therapists are best suited to manage and treat VSS symptoms.
If a patient suspects they have VSS, they can consult VSI’s diagnostic criteria to help achieve an accurate diagnosis. While finding specialists experienced in VSS can be challenging, VSI provides a global list of experts to connect patients with qualified professionals worldwide.
Statistics and Symptoms of Visual Snow Syndrome
Many individuals, especially those born with VSS, may not realize they have a neurological condition, while others may not know their symptoms have a name due to a lack of awareness within the medical community.
The average age of onset is around 29 years, with children often beginning to experience symptoms at approximately 12.5 years, and some cases appearing as early as 8-9 years old.
Visual Snow Syndrome affects about 2-3% of the global population, with no clear prevalence based on gender. It can be present from birth or develop at any time in life, as experienced by Sierra Domb, founder of the Visual Snow Initiative
The primary symptom of VSS is visual snow, a persistent static or dynamic “snow-like” effect visible in the visual field, even with closed eyes.
VSS is a sensory processing disorder that affects how the brain processes visual and non-visual stimuli.
Visual symptoms include afterimages (panilopsia), double vision, trailing phenomena, extreme light sensitivity, floaters (so-called “eye floaters,” 81%), balance issues (55%), convergence insufficiency (nearly 60%), increased entoptic blue field phenomenon (so-called “Scheerer phenomenon”), reduced night vision (68%) and spontaneous flashes of light.
Non-visual symptoms may include tinnitus (60%), migraines (50%), paresthesias (40%), and dissociative experiences such as derealization (where the external world feels dreamlike) and depersonalization (a detachment from oneself).
Not only is migraine a very common phenomenon, but it is also a condition with much comorbidity that probably also shares common pathological mechanisms with visual snow, a topic covered extensively by Puledda et al.5.
More statistics on VSS are available on the Visual Snow Statistics page.
Treatments of visual snow syndrome
The ultimate goal of the research is to deepen the understanding of VSS and find a cure.
In the meantime, VSI is exploring treatment options that may offer symptom relief, especially for those suffering from debilitating forms of VSS.
Drug therapy
Pharmaceutical treatment for VSS has had limited success and, in many cases, has worsened the primary symptom of visual snow.
A 2019 study6 evaluated therapeutic options for a retrospective series of 58 patients, 47 of whom had Visual Snow Syndrome.
Among the medications used, the antiepileptic drug lamotrigine resulted in partial symptom remission in about 20% of patients, but adverse effects, including allergic reactions and daytime drowsiness, were reported in half the cases.
Valproate, acetazolamide, and flunarizine showed no significant symptom improvement.
Visual therapy and lenses
Improved visual acuity and reduced symptoms often help reduce patients’ sense of derealization and depersonalization. Color filters, tinted lenses and oculomotor therapy have provided symptom relief for some patients with VSS. Commonly used filters include yellow-blue spectrum, BPI-Mu, BPI-Omega and FL-41.
Gradual exposure to visual stimuli and training the brain and eyes to process incoming information without being overwhelmed may help some individuals filter symptoms over time.
Mindfulness-Based Cognitive Therapy
Clinical research has shown that Mindfulness-Based Cognitive Therapy (MBCT) may help regulate brain network dysfunctions, particularly in the salience network and vision-related areas.
Additionally, prioritizing nervous system regulation, adequate sleep, and managing sensory overload and stress is crucial for reducing symptom severity and preventing flare-ups.
Each case is unique, and the best approach depends on the patient’s specific symptoms, severity, medical history, and preferences.
We strive to make treatment options accessible”-Sierra Domb explains-“so that patients can choose and work with qualified medical professionals to determine what works best for them. The Visual Snow Initiative website offers more information on treatment options supported by scientific research, tips and resources to help patients and physicians manage VSS
Neuro-visual treatment
In 2022, a study7 by Dr. Charles Shidlofsky, Dr. Terry Tsang, and Vanessa Mora, to evaluate whether neuro-optometric rehabilitation (NORT) can be effective in treating visual snow syndrome in order to improve patients’ quality of life.
NORT is a set of neurosensory and neuromuscular exercises prescribed and supervised by a vision specialist in order to improve oculomotor function, speed, accuracy, visual skills, and processing8.
Visual function of each patient was tested at the start of treatment, at 6 weeks and at 12 weeks after therapy. Twenty-one participants completed the study.
The following visual functions were assessed:
- visual acuity
- ocular motility
- fixation
- pursuit (visual pursuit)
- Saccadic movements by eye-tracking
- accommodation and accommodative flexibility with flipper
- convergence
- fusion amplitudes
- Binocular vision and sensory integration.
The treatment consisted of 12 individual sessions lasting 60 minutes each. Each session included 3-5 exercises to be performed either in the office or at home. The activities were individualized for each patient.
It could be shown at both 6 weeks and 12 weeks that the neuro-visual treatment improved the patients’ quality of life. This improvement occurred in work, study and social life.
The results of this research provide vital information for all health care providers who come across patients with VSS, offering them an effective treatment option. This study justifies the idea that neuro-visual treatment in patients with VSS deserves further investigation.
The future of Visual Snow Syndrome, according to Visual Snow Initiative
The Visual Snow Initiative’s goals are now to expand research, improve access to treatments and ultimately find a cure. The organization is collaborating with top neurologists, neuro-ophthalmologists and researchers to deepen understanding of VSS, develop safe and effective treatments and increase global awareness. The international research team continues to offer scientifically supported treatment options to provide relief while working toward a long-term cure.
My journey with VSS was an unrelenting struggle, plagued by debilitating symptoms, dismissive doctors, and isolation. I channeled my frustration into action and founded VSI to help others by providing the resources I desperately needed at that time.
I hope more physicians will join the cause and use VSI’s resources to improve patient care and symptom management.
– Sierra Domb
The new VSI 4 Kids, an extension of the VSI, provides valuable support for children, parents, teachers, and physicians in understanding and managing VSS in young patients
With continued support, VSI can make further strides in awareness, education, resources, research, and treatment.
Acknowledgements
The editorial team of Emianopsia sincerely thanks the Visual Snow Initiative and, in particular, Sierra Domb for her valuable contribution to this in-depth analysis.
Sierra Domb is the CEO and founder of the Visual Snow Initiative (VSI) and a specialist in health communication, behavioral sciences, and qualitative data analysis, with a particular focus on neuroscience and complex, lesser-known medical conditions such as Visual Snow Syndrome.
Bibliography
- Carroll FD. Visual Symptoms Caused by Digitalis. Trans Am Ophthalmol Soc. 1944;42:243-9. PMID: 16693349; PMCID: PMC1315130. https://pmc.ncbi.nlm.nih.gov/articles/PMC1315130/
- Schankin CJ, Maniyar FH, Chou DE, Eller M, Sprenger T, Goadsby PJ. Structural and functional footprint of visual snow syndrome. Brain. (2020) 143:1106-13. doi: 10.1093/brain/awaa053
- Grande M, Lattanzio L, Buard I, McKendrick AM, Chan YM, Pelak VS. A study protocol for an open-label feasibility feasibility study of transcranial magnetic stimulation for visual snow syndrome stimulation. Front Neurol. (2021) 12:724081. doi: 10.3389/fneur.2021.724081
- J Ciuffreda, Kenneth, MH Esther Han, Barry Tannen, and Daniella Rutner. 2021. “Visual Snow Syndrome: Evolving Neuro-Optometric Considerations in Concussion/Mild Traumatic Brain Injury.” Concussion 6 (2). doi 10.2217/cnc-2021-0003
- Puledda F, Schankin C, Digre K, Goadsby PJ. Visual snow syndrome: what we know so far. Curr Opin Neurol. 2018 Feb;31(1):52-58. doi: 10.1097/WCO.0000000000000523. PMID: 29140814
- Van Dongen RM, Waaijer LC, Onderwater GLJ, Ferrari MD, Terwindt GM. Treatment effects and comorbid diseases in 58 patients with visual snow. Neurology. 2019 Jul 23;93(4):e398-e403. doi: 10.1212/WNL.0000000000007825. Epub 2019 Jun 18. PMID: 31213497; PMCID: PMC6669936.
- Tsang T, Shidlofsky C, Mora V. The efficacy of neuro-optometric visual rehabilitation therapy in patients with visual snow syndrome. Front Neurol. 2022 Dec 5;13:999336. doi: 10.3389/fneur.2022.999336. PMID: 36545398; PMCID: PMC9760742.
- Sandra M. Fox and Paul Koons and Sally H. Dang. Vision Rehabilitation After Traumatic Brain Injury. Phys Med Rehabil Clin N Am. (2019) 30:171-88. doi: 10.1016/j.pmr.2018.09.001

You are free to reproduce this article but you must cite: emianopsia.com, title and link.
You may not use the material for commercial purposes or modify the article to create derivative works.
Read the full Creative Commons license terms at this page.