Treatments for patients with hemianopia

The term hemianopsia is derived from the Greek: “hemi” (half) + “an” (without) + “opsia” (sight).
By definition, therefore, the term hemianopsia refers to a vision deficit characterized by the impairment of half of the visual field.
The loss of half of the visual field may involve the right or left half (lateral or vertical hemianopsia) or the upper or lower half (altitudinal or horizontal hemianopsia).
Etiology: the causes of hemianopsia
The etiology of this disorder can be attributed to lesions of the optic pathways caused by various pathological conditions.
“Hemianopsia is caused by injury or compression at any level of the optic pathways. In fact, these events can impair the normal transmission of bioelectrical signals from the retina to the visual cerebral cortex.” 1
Most causes are attributable to optic pathway compression: similar to crushing a water pipe, the bioelectric signal no longer passes (or passes only partially) if a nerve or brain area is compressed.
The most common injuries are vascular (ischemia, hemorrhage, aneurysms); neoplastic (e.g., brain tumors), inflammatory, demyelinating, and traumatic injuries can also cause optic nerve compression.
Classification of optic nerve injuries
Hemianopsia can be classified according to the site of the lesion or according to the campymetric deficit.
Lesion site
The image below illustrates the rule of a full-thickness chiasmatic lesion.
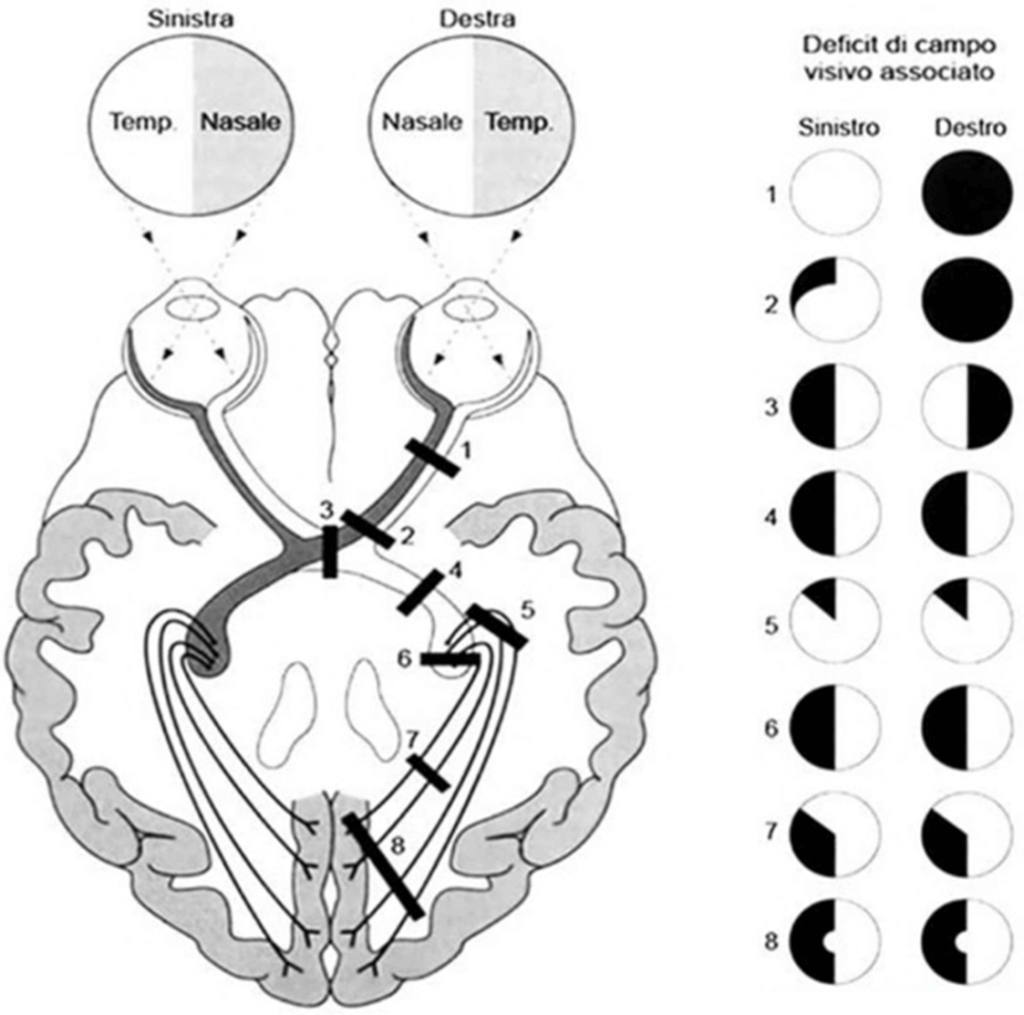
1) Blindness in right eye 2) Blindness in right eye and partial superior temporal quadrantanopia in left eye 3) Bithemporal hemianopsia 4) Left homonymous hemianopsia 5) Left superior homonymous sector deficit 6) Left homonymous hemianopsia 7) Incomplete left homonymous hemianopsia or superiorly extended left inferior quadrantanopia 8) Left homonymous hemianopsia with macular sparing
The lesion can be of three types:
- prechiasmatic: it affects the section of the optic pathways between the eyeball and the chiasm, the point where the optic nerves of both eyes meet and cross part of the fibers. The image describes a blindness of the right eye: the left eye transmits information, the right eye does not. To simplify the explanation, the eye is presented as completely blind (a situation that could occur in the case of a resected nerve);
- chiasmatic: given the space the optic nerve occupies and the size of the chiasm, depending on the cause of the chiasmatic lesion, either the anterior fibers or the posterior fibers could be involved, which could give lesion results that are not always homogeneous;
- retrochiasmatic or postchiasmatic: lesions affecting the nerve pathways between the chiasm and the cerebral cortex; continuing posterior to the optic chiasm, the visual field is lateralized: the two portions (nasal and temporal) move to the same side, this results in an opposite field projection (hemianopsic lesion on the same side of the visual field).
In the final part, when we are in the vicinity of the occipital cortex, the form of hemianopsia we observe involves central (macular) sparing, because the distribution of central fibers is very deep over the cortex and most lesions spare this area.
The crossing (so-called “decussation”) of the two optic nerves at the level of the optic chiasm results in the projection of information (image) from the right visual field onto the left optic nerve and vice versa. Fiber distribution thus allows lateralization (differentiation by nerve structure or function), binocular vision, and area sparing: fiber distribution allows a lesion not to involve the whole nerve; if the optic nerve were compact as it is at the orbital level, the final effect would be immediate blindness in any nerve tract.
Decussation and lateralization prevent extensive damage.
Campymetric deficit
Hemianopias are distinguished into:
- homonymous if they affect the same side of the visual field (loss of either the outer two halves of the visual field, i.e., bitemporal, or the inner halves, i.e., binasal)
- heteronymous if they affect opposite sides of the visual field (loss of the left or right halves of the visual field).
Diseases associated with hemianopsia
Diseases that can be associated with hemianopsia are as follows (list is indicative and not exhaustive):
- Carotid aneurysm
- Cerebral aneurysm
- Stroke
- Cerebral ischemia
- Transient ischemic attack (TIA)
- Cerebral hemorrhage
- Meningitis
- Trauma
- Brain tumors
- Tumors of the pituitary gland
- Multiple sclerosis
Special types of hemianopsia
Temporary hemianopsia
It is important to make a distinction between permanent and temporary hemianopsia.
Temporary hemianopsia is not necessarily indicative of an anatomic lesion and may occur, for example, during a migraine visual aura.
Neglect
Neglect is a neuropsychological syndrome characterized by the patient’s inability to perceive or pay attention to objects, people, representations, located in a visual hemicampus (usually contralateral to the lesion) and to act in that side of space.
For further study, we recommend reading from Neglect: what it is, how to recognize it, how to treat it.
Quadrantanopia
Finally, there is also the possibility of quadrantanopia or quadrant hemianopsia, which is the loss of only one quadrant of the visual field.
Although quadrantanopia is not assimilated to the definition of hemianopsia, it should be remembered among the symptoms of optic tract lesions and entered into a classification.
Implications for everyday life
Injuries to the optic pathways result in impairment that can cause disability and handicap.
The patient may experience problems with mobility and orientation.
A large number of people with field deficit report difficulty in:
- going down stairs
- grasping objects
- coordinating eye-motor movements, due to the frequent associated loss of three-dimensional vision.
Note that if the macular region is involved, the patient will also have difficulty with reading and writing activities.
More information on psychological aspects will be covered in future articles.
Instrumental diagnostics and therapy
Campimetric assessment (visual field) allows us to make an approximate diagnosis of the site of the lesion.
The therapeutic approach varies, of course, depending on the recognized cause: for example, in the case of a tumor, surgical removal of the tumor may be performed, while in the case of an aneurysm, vascular neurosurgery may be used.
If nerve cell death of the optic pathways has not already occurred, it is likely that after surgery, the condition of hemianopsia will be just a bad memory.
Unfortunately, in some cases, even if such surgery is performed, the damage is irreversible and it is therefore impossible to “recover” the lost portion of the visual field.
Rehabilitation of hemianopsia
Rehabilitation plays an important role in visual recovery.
Studies on perceptual learning show that setting up a propaedeutic environment to stimulate the affected side, i.e., positioning bed, chairs, table so that the patient holds conversations and treatments from the affected side, are valid rehabilitation therapies.
The improvement of vision in the affected half of the field follows a sequence that begins with light perception and continues with motion perception, then shape perception, and finally color perception.
There are three types of hemianopsia rehabilitation, all characterized by constant repetition of visual exercises:
- optical therapy
- eye-movement therapy
- vision restoration therapy (VTR)
The first two (optical and eye-movement therapy) seek to compensate for the visual field deficit, the third to recover it (vision restoration therapy).
Changes in neuronal activity have been described in patients with hemianopsia following ischemic injury to the visual cortex. This reorganization may facilitate compensation for lost visual function that is rarely fully restored.
It has been shown that enhancement of exploratory eye movements with appropriate training can compensate for visual-perceptual impairment during activities of daily living.
Dual visual and auditory stimulation offers possibilities for recovery not achievable with systems based on optical therapy alone.
Clinical studies of more than 200 patients, including non-cooperating patients, have demonstrated a doubling of the visual abilities of patients with hemianopsia with 1 hour per day non-continuous therapy, in as little as 20 days. An average increase in the patient’s reading speed of 50% was demonstrated in these cases and up to 100% after 4 months. This improvement remains stable over time. 12
Bibliography
- IAPB Italy – International Agency for the Prevention of Blindness (https://iapb.it/emianopsia/#:~:text=La%20maggior%20parte%20delle%20cause,segnale%20passa%20solo%20in%20parte)
- Training Cognitivo: Neglect: il lato oscuro del mondo (https://www.trainingcognitivo.it/neglect-il-lato-oscuro-del-mondo/)
- Visual impairment following stroke: do stroke patients require vision assessment? Age and Ageing, Volume 38, Issue 2, March 2009 (https://academic.oup.com/ageing/article/38/2/188/16402)
- V isual Field Defects after Stroke: A Practical Guide for GPs. Australian Family Physician (https://search.informit.org/doi/abs/10.3316/INFORMIT.190560378671632)
- La riabilitazione dei deficit centrali di campo visivo (https://www.researchgate.net/publication/294889236_La_riabilitazione_dei_deficit_centrali_di_campo_visivo)
- Eye-movement training-induced plasticity in patients with post-stroke hemianopia (https://link.springer.com/article/10.1007/s00415-009-5005-x)
- La riabilitazione visiva dell’emianopsia: dal training psicofisico alla stimolazione elettrica (https://thesis.unipd.it/handle/20.500.12608/29454)
- Developmental Eye Movement Test: reliability and symptomatology (https://pubmed.ncbi.nlm.nih.gov/16038866/)
- Vision Restoration Therapy (VRT) Efficacy as Assessed by Comparative Perimetric Analysis and Subjective Questionnaires (https://content.iospress.com/articles/restorative-neurology-and-neuroscience/rnn00297)
- Fondazione Veronesi: Ictus cerebrale, la riabilitazione per recuperare la vista (https://www.fondazioneveronesi.it/magazine/articoli/neuroscienze/ictus-cerebrale-la-riabilitazione-per-recuperare-la-vista)
- Treccani: quadrantopsia (https://www.treccani.it/enciclopedia/quadrantopsia_%28Dizionario-di-Medicina%29/)
- Visual search improvement in hemianopic patients after audio-visual stimulation (https://academic.oup.com/brain/article/128/12/2830/420505)

You are free to reproduce this article but you must cite: emianopsia.com, title and link.
You may not use the material for commercial purposes or modify the article to create derivative works.
Read the full Creative Commons license terms at this page.