Nystagmus and Audiovisual Stimulation: a new approach in Neurorehabilitation

Nystagmus: a clinical challenge
Nystagmus is an oculomotor disorder characterized by involuntary eye movements that can impair visual stability and balance. There can be many causes, from neurological disorders to vestibular dysfunction to congenital conditions. This disorder is often associated with oscillopsia, an unstable visual perception that significantly reduces patients’ quality of life.
Currently available rehabilitation options offer variable results, and often do not guarantee lasting improvements. Traditional strategies such as fixation exercises, optical compensation and the use of prismatic lenses can provide some degree of benefit, but they do not always provide effective long-term control of the disorder.
However, new approaches based on multisensory stimulation are emerging as possible strategies to optimize the management of this condition.
An innovative approach to the problem
In Italy, an audiovisual stimulation protocol has been developed at the Neurorehabilitation Unit, Azienda Ospedaliera Universitaria Pisana (AOUP) with the aim of improving ocular and postural stability in patients with nystagmus. This approach is based on the integration of visual and auditory stimuli to promote better motor and perceptual control.
The scientific rationale for this methodology is based on the principles of brain plasticity and multisensory integration. The brain, exposed to coordinated stimuli between vision and hearing, can reorganize neural connections to improve spatial perception and control of involuntary eye movements.
Recent studies suggest that this type of stimulation may promote neural adaptation and improve the compensatory capacity of the central nervous system.
A Clinical Case Study: audiovisual stimulation in FXTAS syndrome
In the Case Study published in December 2024 in ScienceDirectt1, a 60-year-old female patient, diagnosed with progressive nystagmus associated with FXTAS syndrome (fragile X-related tremor/ataxia), presented with postural instability, oscillopsia, and difficulty walking. These symptoms significantly impaired his autonomy, making even the simplest daily activities difficult.
To deal with these problems, a customized rehabilitation protocol including 30 sessions of audiovisual stimulation, proprioceptive exercises and muscle strengthening was applied.
The goal of the treatment was to improve ocular motor control and postural stability through modulation of sensory input.
The pre and post-treatment analysis was conducted by means of a medical device for multisensory stimulation and methods such as microperimetry2 to assess eye fixation.
Fine motor skills and balance were measured with functional tests, including:
- Timed Up and Go3 (measures the time taken to get up from a chair, walk, turn around, and sit back down)
- 10-meter walk test4 (measures average walking speed in meters per second)
- Berg Balance Scale5 (fall risk assessment scale)
These measures made it possible to objectively quantify the patient’s progress during rehabilitation.
Outcomes, clinical implications
At the end of treatment, the patient showed significant improvement in ocular fixation stability and a reduction in visual symptoms, such as oscillopsia. Functionally, increased confidence in walking and increased autonomy in daily activities were observed.
An attractive aspect was the maintenance of the benefits over time: six months after the end of treatment, improvements were still evident, suggesting that audiovisual stimulation may promote stable neural adaptation.
Follow-up at 6 months indicated continued improvements in performance from baseline, particularly in terms of success rates and response times in sessions conducted without drug administration (see Figs. 1 and 2).
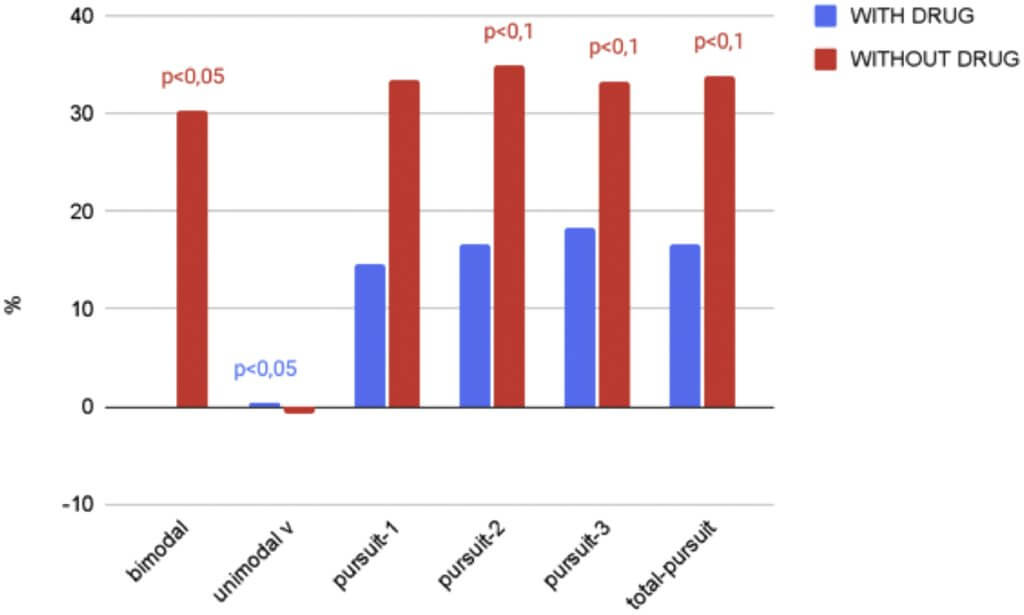
with and without drugs (Fampridine). From baseline to 6-month follow-up1.
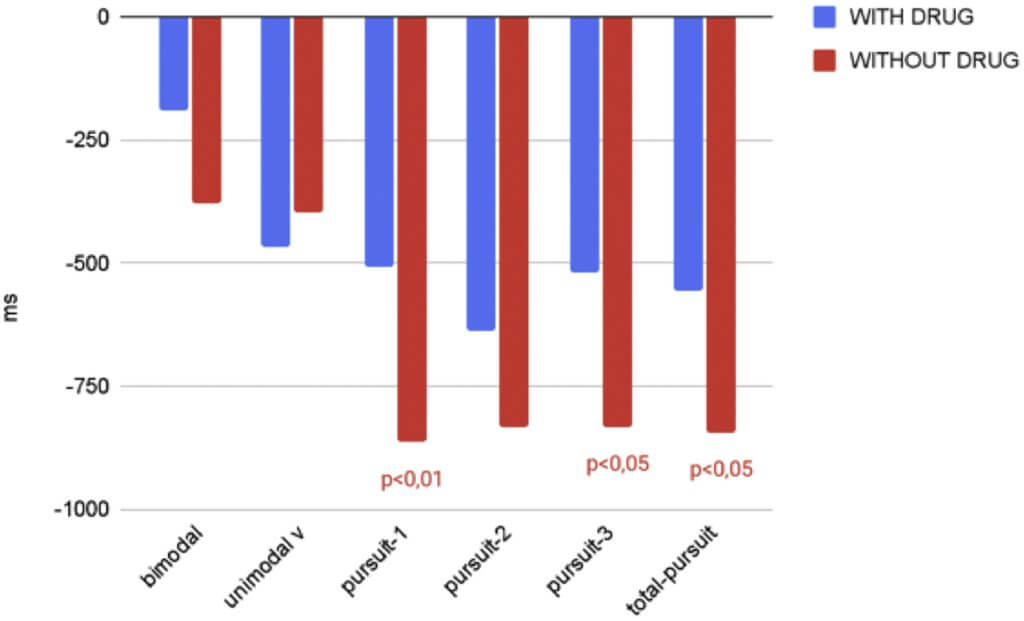
with and without drugs (Fampridine). From baseline to 6-month follow-upi1.
Future perspectives
This achievement opens promising prospects for the use of this technique in the treatment of other neurological disorders with impaired ocular motor control.
Audiovisual stimulation represents an innovative rehabilitation option for patients with nystagmus and other ocular motility impairments. Integration of this technique with other strategies, such as virtual reality and other neuromodulation methods, could expand therapeutic possibilities and further improve clinical outcomes.
The Italian AOUP Neurorehabilitation experience shows that optimizing sensory input can lead to real and lasting improvements in the management of nystagmus. The ability to harness brain plasticity to promote better motor and visual control represents an important opportunity for neurological rehabilitation.
These preliminary results show that audiovisual stimulation improves the quality of life of patients with oculomotor and postural disorders, opening new therapeutic perspectives in neurorehabilitation.
Bibliography
- Damiano Antognetti, Luca Maggiani, Elena Gabbrielli, Luca Allegrini, Stefania Dalise, Carmelo Chisari. Neurovisual Training With Acoustic Feedback: An Innovative Approach for Nystagmus Rehabilitation, Archives of Rehabilitation Research and Clinical Translation. Volume 6, Issue 4, 2024, 100371, ISSN 2590-1095. Doi: 10.1016/j.arrct.2024.100371.
- A Molina, RJ Pérez-Cambrodì, P Ruiz-Fortes, C Laria, DP Piñero. Utility of microperimetry in nystagmus: a case report. Can J Ophthalmol, 48 (2013), pp. e103-e105. Doi: 10.1016/j.jcjo.2013.07.017.
- Killough, J.. VALIDATION OF THE TIMED UP AND GO TEST TO PREDICT FALLS. Journal of Geriatric Physical Therapy 29(3):p 128-129, December 2006. Doi: 10.1519/00139143-200612000-00034.
- Rahman, M., & Alagappan, T. R. (2019). The test–retest reliability of 10 meter walk test in healthy young adults-A Cross sectional study. IOSR J Sports Phys Edu, 6(3), 1-6.
- Katherine Berg, Sharon Wood-Dauphine, J.I. Williams, and David Gayton. Measuring balance in the elderly: preliminary development of an instrument. Physiotherapy Canada 1989 41:6, 304-311. Doi: 10.3138/ptc.41.6.304.

You are free to reproduce this article but you must cite: emianopsia.com, title and link.
You may not use the material for commercial purposes or modify the article to create derivative works.
Read the full Creative Commons license terms at this page.



